|
Background
Breast cancer is the most common cancer form among western
women. Traditionally there have been the individual woman's
responsibility to examen her breast and contact her physicist when
something suspicious is felt. A disadvantage with this approach is
that the cancer has often grown too large before discovery so the
long time survival rate for patients are rather low. This makes it evident that a
method that makes an earlier detection of breast cancer possible is
needed. Today this method is screening with mammography.
Screening
A screening is defined as the "presumptive identification of
unrecognized disease or defect by application of tests, examinations,
or other procedures which can be applied rapidly". In the case of
breast cancer the Swedish Socialstyrelsen (health board) recommend
the following:
The screening should be performed with mammography with a
resolution of 15 line-pairs per millimeters,
The mammograms should be judged by two radiologists independent of
each other,
Women should be called to have their breast X-rayed every second
year from the year they turn 50 and until the year they turn 69.
From above can be seen that the screening produces a lot of images
that must be judged. If some sort of computer aid could be introduced
large economical gains could be expected.
Aim
The aim with this project is to develop methods which in the long run
enables the implementation of a prototype system for
computer aided mammographic screening. This system will be evaluated
with respect to:
Medicine: It is expected that some new relationships between a
person and her probability to develop breast cancer will be
found. This is due to the fact that large data sets will be examined
in order to find a better screening base.
Public health: It will be examined if it is possible to use an
individual calling frequency in the screening process. If this is
possible will the public health increase, since the persons that have
a greater probability to develop breast cancer will be monitored more
closely.
Economical: A successful system would make it possible to remove
one radiologist from the judging process.
Pedagogical: There are a shortage of trained radiologists in
mammography that may teach new radiologists. With a system of this kind
it would be possible to let new radiologists do their initial training
with the system.
Computer Scientific: Within this project will new computer
scientific theories specially with in the field of image processing be
developed. A concrete example of this is a metric topology for images.
Medical Informatics: This is an initial project at the department
of computing science within the field of medical imaging. The
experience gained within this project will make it possible to define
and carry through more advanced projects in the future.
Methods
Our approach to solving this problem is not to focus on specific
techniques or methods, but to analyze the problem area thoroughly and
then solve the different sub-problem identified.
Overall Methods
By parameterize the screening process we will gain an understanding of
the problem area and make it possible to reason about where in the
process different computer aid will be suitable. From this formalism
it is also possible to conclude what kind of knowledge that are needed
for the different steps of the implementation. After this
understanding has been formed the outline of the system may be
drawn.
References
- F. Georgsson, Algorithms and Techniques for Computer Aided
Mammographic Screening, Ph.D. thesis, Umeå University, UMINF-01.15, 2001
- F. Georgsson and P. Eklund,
An Identification of Handling
Uncertainties Within Medical Screening: A case study within
screening for breast cancer, In: H .N. Teodorescu,
A. Kandel, and L.C. Jain (editors), Applications of Fuzzy &
Neuro-Fuzzy Systems in Medicine and Bio-Medical Engineering
, CRC-press, 1998
- F. Georgsson, and S. Carlson.
A framework for computer aided mammographic screening,
in N. Karssemeijer, M. Thijssen,
J. Hendriks, and L. v. Erning (editors) Digital
Mammography, Kluwer Academic Press, 1998
- F. Georgsson, Computer Aided Mammography. A study of the
possibilities of building a mammographic expert system, Master's Thesis, Umnad-161.96, Umeå University
Specific Methods
In the previous section it were described how we approached the
problem top down, not concentrating on specific methods. However it is
clear that we can not implement a useful system using this approach, at
least not within reasonable time frames. Hence, we must combine the top-down approach with a bottom up.
Image Registration
A screening mammogram is intended to capture the signs of breast
cancer before the cancer has had the change to spread to vital
organs. This implies that in the most cases the signs of breast cancer
are very subtle in a screening mammogram and hence rather hard to
find, which is the motivation for double judging of screening
mammograms. The most effective way to detect these subtle changes is
to compare the current mammogram both with previous images of the same
breast (temporal comparison) or images of the corresponding
breast (bilateral comparison).
We have developed methods to registered, that is find corresponding
features in two mammograms, and transform the images to enable the
computer to compare images automatically. When the images are aligned
with each other it is possible to find asymmetrical developments by a
rather straightforward image subtraction procedure. Publications 8 and
12, see below, describes this techniques in more detail and examples
of images are seen in figure 1 and figure 2.
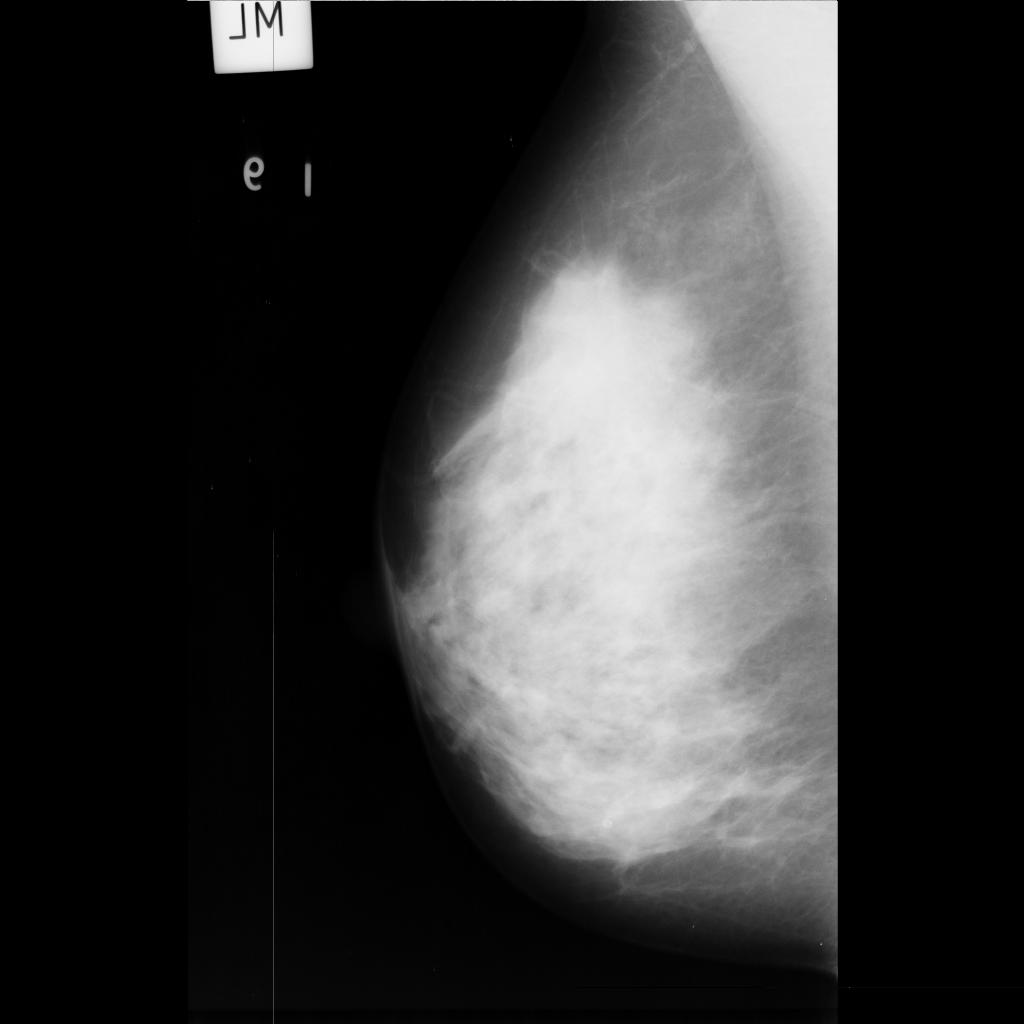
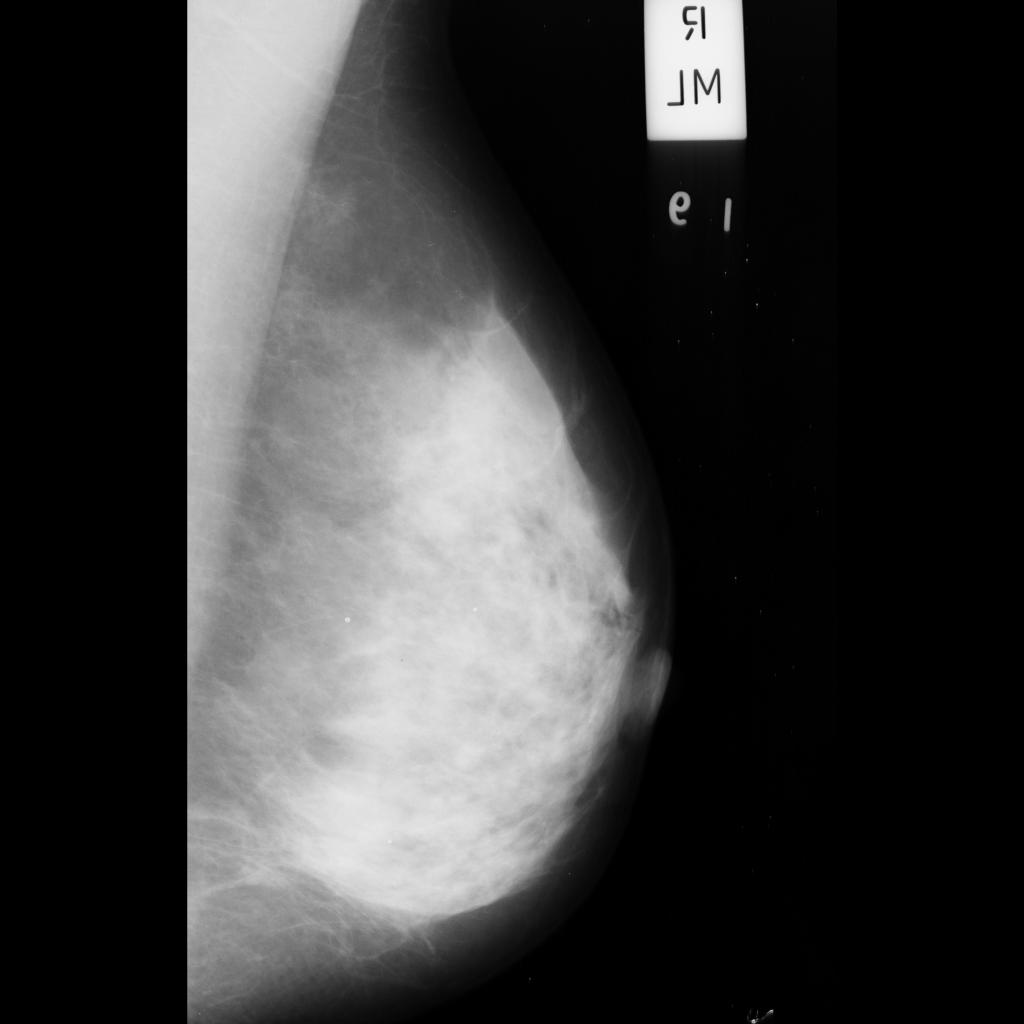
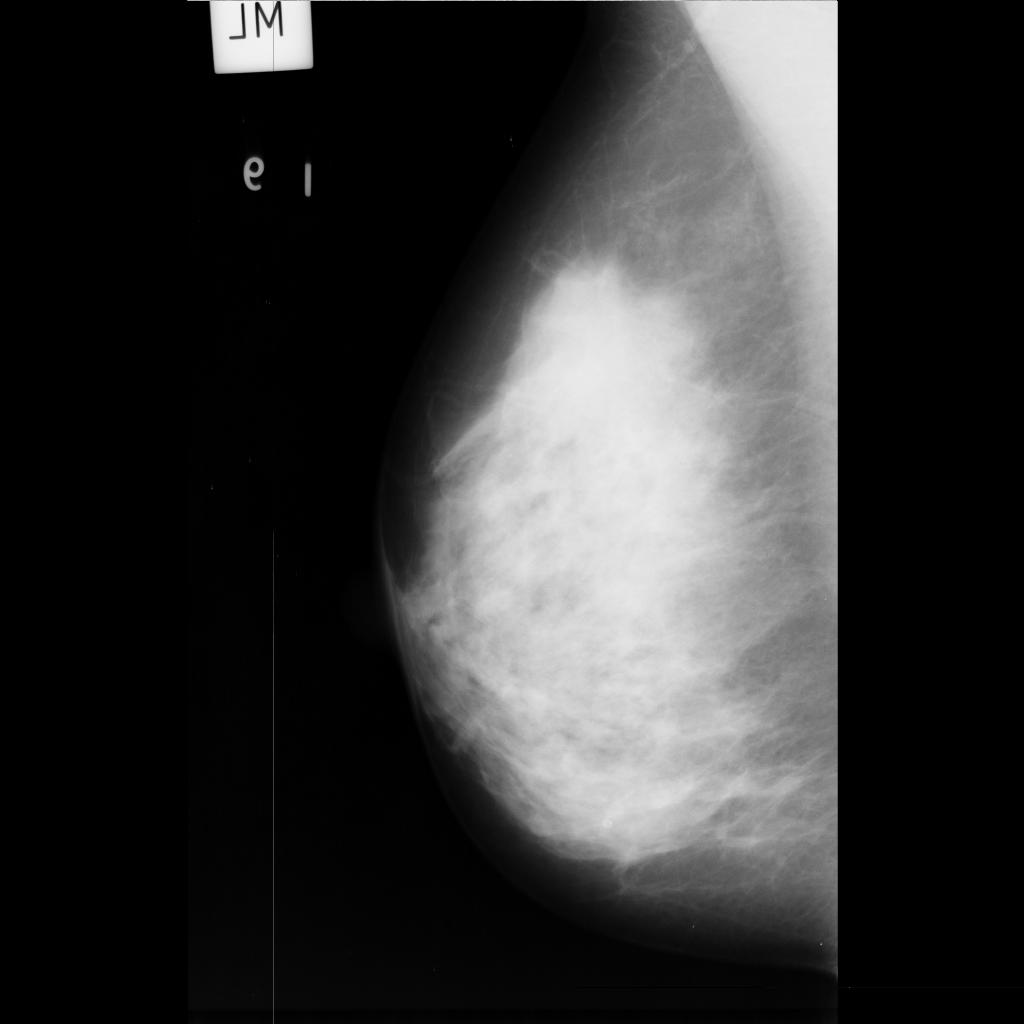
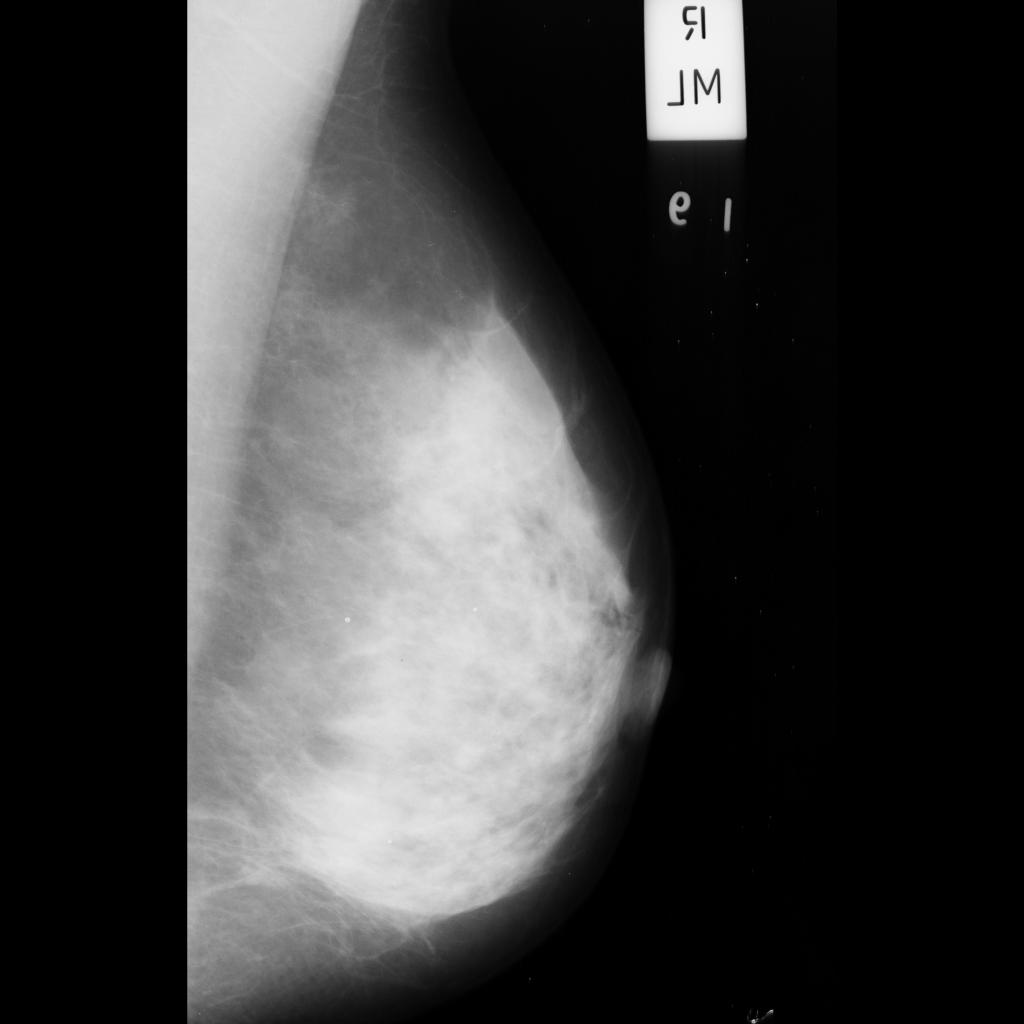
Figure 1. Original mammograms. Observe the difference in size and shape
between the two breasts
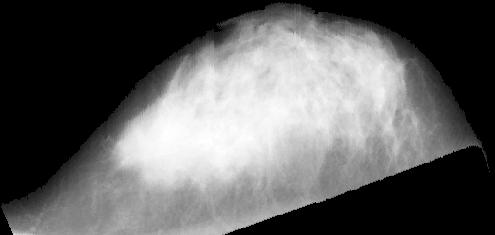
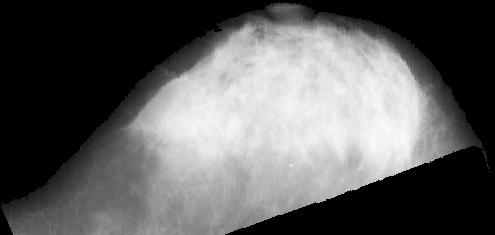
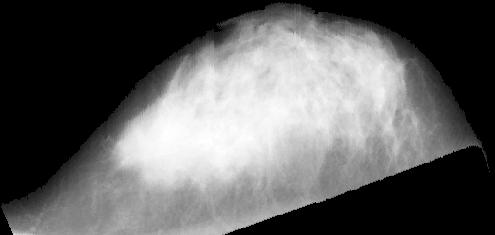
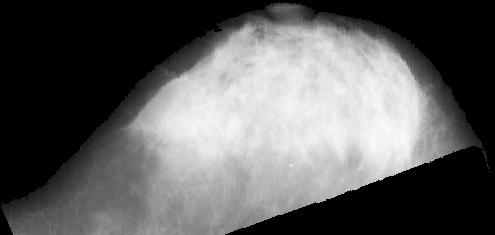
Figure 2. Registered and transformed mammograms. The images of the two
breasts are now the same size and shape and the nipple and pectoralis
muscle are aligned.
References
- C. Olsén and F. Georgsson, Problems Related to Automated Nipple Extraction, in H. Kalviainen, J. Parkkinen and A. Kaarna (eds), SCIA 2005, LNCS 3540, Springer Verlag, pp. 470-480, 2005
- C. Olsén, On the problem of Extracting the Breast Border and Mamilla from Mammograms, in E. Bengtsson and M. Eriksson (eds) Proc. of SSBA '04, pp 154-157, 2004
- F. Georgsson, Differential analysis of bilateral mammograms, International Journal on Pattern Recognition and Artificial Intelligence, Vol. 17, No 7, pp. 1207-1226, 2003.
- C. Olsén, and F. Georgsson The Accuracy of Geometric Approximation of the Mamilla
in Mammograms, in H.U. Lemke, M.W. Vannier, and K. Inamura, A.G. Farman, K. Doi, and
J.H.C. Reibner (eds) Computer Assisted Radiology and Surgery, Excerpta Medica ICS 1256, pp.
956-961, 2003
- F. Georgsson Anatomical coordinate system in bilateral registration of
mammograms, in J. Bigun and T. Gustavsson (eds) SCIA 2003, LNCS 2749, Springer Verlag,
pp. 335-242, 2003
- F. Georgsson, A Novel Method for Direct Bilateral Comparison of
Mammograms, In proceedings of SSAB '02, Lund, March 7-8, 2002.
- F. Georgsson, On the problem of Bilateral Comparison of
Mammograms, in proceedings of IWDM 2002
- F. Georgsson, Differential Analysis of Bilateral
Mammograms, Technical Report UMINF-01.14, 2001.
- F. Georgsson, A Novel Approach to Finding Corresponding Points in
Bilateral Mammograms, Technical Report UMINF -01.13, 2001.
- F. Georgsson, Differental Analysis of Bilateral
Mammograms, In I. Austvoll (editor), proceedings of SCIA-2001, pp 70-77, 2001
- F. Georgsson Transformation of Mammograms based on Anatomical
Features in M. Yaffe (editor) proceedings of International Workshop on
Digital Mammography, pp. 721-726, 2000.
- F. Georgsson, Transformation of Mammograms Using Anatomical
Features, Presented at the 11th Scandinavian Conference on
Image Analysis, Kangerlussuaq, Greenland, June 7-11, 1999
Compression Modelling
A mammogram is an x-ray image of a female breast. Like all x-ray images, the intensity in a point corresponds to the accumulated attenuation of the x-rays along a line through the image point and the x-ray foci. In order to minimise the dosage for the woman and optimise the image quality the breast is compressed when the image is acquired. The effects of the compression makes it very hard to determine what points in the uncompressed breast that are projected onto a specific image point. If the tissue movement inside the breast while under compression could be modelled, it would be possible to calculate, for instance, three-dimensional coordinates based on the images taken from different angles. When combined with models for anatomical symmetry it would also allow for a sound approach to bilateral comparison of mammograms, one of the key issues in incorporating domain specific knowledge into computer aided judging of mammograms. In other words, it could be argued that breast compression modelling is one of the most important fields within modern mammographic image processing.
References
- F. Georgsson, and N. Björnestål, On the Problem of Breast
Compression Modelling, Technical Report UMINF 01.20, Presented
at CARS 2002, Paris, June 26-29.
- N. Björnestål, On the Subject of Breast Compression Models for X-ray Mammography, Master's Thesis, UMNAD-381/02, Umeå University, 2001
- F. Georgsson, Multi view 3 dimensional reconstructions of points in mammograms in proceedings of SSAB symposium, pp. 41-44, 2001
Automatic Determination of Mammogram Adequacy
There are several problems involved in the quality assessment. First, it
must be fully understood what is meant with a 'good quality mammogram'.
Furthermore, there might be differences between the quality criteria in
different countries. One example of this is that in Sweden the MLO is
taken at an angle of 60 degrees but in the UK and the Netherlands the
angle is defined in terms of the length of the woman (the images should be
taken from shoulder to opposite hip). This clearly affects the appearance
of the breast on the mammogram and thus changes the quality criteria for a
good mammogram. The first step is to investigate the quality criterion
both as described in the literature and by interviewing radiologist that
judges screening mammograms on a daily basis. The quality criteria will be
formulated in linguistic terms. For example: The parenchyma should be well
spread.
The next step is to quantitatively describe the linguistic
variables of the qualitative criterion. What does a radiologist mean by
the term 'well spread'? By using fuzzy logic in describing the system of
quality rules, it is possible to model the linguistic variables.
The
hardest part, however, is to model the cognitive ability of the
radiologist. That is to be able to distinguish between different tissue
types, such as fat and glandular tissue (parenchyma).
References
- C. Olsén Automatic Determination of Mammogram Adequacy - A Holistic Approach, to appear in Digital Mammography 2004
- C. Olsén Anatomical landmarks considering adequate mammograms, in C. Rother and S. Carlsson, Proceedings of SSAB'03, pp. 29-32, 2003
- C. Olsén Automatic evaluating the curvature of the pectoralis muscle in
mammograms, in J. Bigun and T. Gustavsson (eds) SCIA 2003, LNCS 2749,
Springer Verlag, pp. 446-453, 2003
- C. Olsén, Automatic Determination of Mammogram Adequacy, Masters Thesis, UMNAD 424/02, 2002
Image Metrics
A large number of problems within medical imaging is to compare an
image, or part of an image, to a reference image showing certain signs
of a disease. The difference between the images is then the base for the
diagnose, or as in screening, the selection. From this it is evident
that an image-metric would be useful, and such a metric has been
developed.
The metric itself does not solve all the problems that may arise in
solving a medical imaging problem. Some sort of transformation is also
needed, examples of such transformations are: wavelets or SGLD
(Spatial Gray-Level Dependencies) for transforming an image to a
texture specific space. In this space may the metric be applied.
References
- F. Georgsson, Evaluation of texture metrics, Presented
at Pattern Recognition in Practice VI, Vlieland, The
Netherlands, June 2-4, 1999
- P. Eklund, and F. Georgsson, Unraveling the Thrill of Metric Image
Spaces, in G. Bertrand, M. Couprie, and L. Perroton
(editors), Discrete Geometry for Computer Imagery, LNCS 1586,
Springer, 1999.
- F. Georgsson and P. Eklund,
A metric framework for texture measurements, In
Proceedings of SSAB '98, March 16-17, 1998, Uppsala,
Sweden.
Tissue Classification
To use anatomical knowledge of the domain expert more efficiently it is
important to be able to divide the image of the breast into anatomical
zones describing different tissue types. One way of achieving this is to calculate the fractal dimension of the projected tissue.
References
- F. Georgsson, P. Wingren, and A. Nilsson, Problems Related to Determining the Fractal Dimension of Tumors in X-Ray Images, Presented at Fractal 2004, Vancouver, Canada, April 4-7, 2004
- P. Wingren, F. Georgsson, and A. Nilsson, Some Families of Mathematical Fractals and Projections, Lower Box-, Upper Box- and Hausdorff Dimensions, Presented at Fractal 2004, Vancouver, Canada, April 4-7, 2004
- F. Georgsson, Fractal dimensions and the geometry of x-ray imaging, In E. Bengtsson and M. Eriksson (eds), Proceedings Symposium on Image Analysis, pp. 150-153, Uppsala, March 11-12, 2004
- F. Georgsson, On the problem of why it is hard to determine the fractal dimension of medical images?, In C. Rother and S. Carlsson, Proceedings of SSAB '03, pp. 69-72, KTH, March 6-7.
- F. Georgsson, and G. Hoppe On the problem on tissue
classification in mammograms in H.U. Lemke, M.W. Vannier,
K. Inamara, A.G. Farman and K. Doi (editors)
CARS 2000, pp. 741-746, Elsevier Science B.V., 2000
- F.Georgsson, and G. Hoppe Towards a more human way of judging
screening mammograms automatically, In H.R. Arabnia (editor)
Proceedings of The International Conference on Imaging
Science, Systems, and Technology (CISST'99), Las Vegas,
1999, pp 257-263.
- G. Hoppe, Dividing Mammograms into Anatomical Zones, Master's
Thesis, Umeå University 1999.
Detection of Microcalcifications by Wavelet Methods
Automatizing the detection of microcalcifications in mammographic images
is a difficult task, mainly due to the nature of the mammograms. The
mammograms are images of high resolution and low contrast. There is also a
great variation in the grayscales of different mammograms. In some
mammograms the calcifications are visible as nearly white spots on a dark
gray background, while they in other mammograms are visible as brighter
gray spots on a slightly darker gray background. There may also be other
bright regions not associated with calcifications, which makes straight
forward thresholding methods unsuitable for extraction of calcifications.
Several different wavelet based approaches to the problem of extraction of
microcalcifications can be found in the literature. However, they all have
in common the utilization of the fact that calcifications in general are
small, and that they therefore appear in certain levels of the wavelet
decomposition of the image.
References
- A. Söderström, Using
Wavelet Methods to Extract
Microcalcifications in Mammograms, Master's Thesis,
UMNAD-197.97, Umeå
University
Results
The project has so far resulted in the publications listed after each
area. The following theses have also been produced within the project
- C. Olsén, Automatic Assessment of Mammogram Adequacy, Licentiate Thesis, UMINF-05.15, 2005
- C. Olsén, Automatic Determination of Mammogram Adequacy, Masters Thesis, UMNAD 424/02, 2002
- N. Björnestål, On the Subject of Breast Compression Models for X-ray Mammography, Master's Thesis, UMNAD-381/02, Umeå University, 2001
- F. Georgsson, Algorithms and Techniques for Computer Aided
Mammographic Screening, Ph.D. thesis, Umeå University, UMINF-01.15, 2001
- F. Georgsson Computer Aided Medical Imaging with Applications
in Mammographic Screening, Licentiate Thesis, UMINF-99.06,
1999.
- G. Hoppe, Dividing Mammograms into Anatomical Zones, Master's
Thesis, Umeå University 1999.
- A. Söderström, Using
Wavelet Methods to Extract
Microcalcifications in Mammograms, Master's Thesis,
UMNAD-197.97, Umeå
University
- F. Georgsson, Computer Aided Mammography. A study of the
possibilities of building a mammographic expert system, Master's Thesis, UMNAD-161.96, Umeå University
Funding
The project was
up to 1998 funded by the county council of Västerbotten and through the Cooperative Health Information Network (CHIN) project.
Work on the problem of tissue classification by using fractal methods is funded by the Swedish Research Council (Vetenskapsrådet) and the Faculty of Science and Technology, Umeå University,
Work on automatic determining the adequacy of mammograms is funded by the Department of Computing Science.
Parts of the work is carried out within the Centre for Biomedical Engineering and Physics.
-
Contacts
- Fredrik Georgsson, Ph.D.
(Umeå University)
- Christina Olsén, M.Sc. (Umeå University)
- Stina Carlson, M.D. (Chief Radiologist, University Hospital
of Northern Sweden, Mammographic Unit)
|